A patient’s own salvaged red blood cells (autologous red blood cells) are functionally superior to donated red blood cells. This is the first out of seven reasons why autologous blood should be considered the preferred source of blood supply.
Refrigerated storage of blood results in changes in the red cells. This alters their function, the phenomenon is referred to as storage lesions.
Upon leaving the bloodstream the supply and disposal of substances required for red blood cell survival is disrupted. If remaining outside of their natural environment for a longer period of time. The blood cells suffer oxidative damage due to lack of sufficient oxygen. In addition, waste products start to accumulate while the nutritional supplies become depleted.
As a result, donated red blood cells could change shape and become deformed. Their metabolism could be deranged and vital parts in the cell may sustain oxidative injuries. Luckily, extensive efforts to prevent the red cells from completely losing the ability to bind and deliver oxygen have paid off.
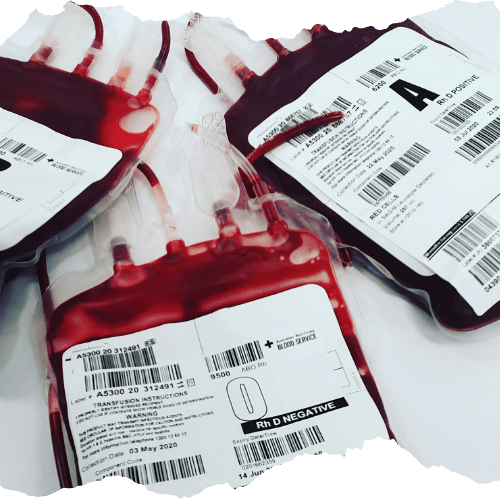
Since blood component separation became the mainstay of donor blood banking. So-called additive solutions have been used to prolong red blood cell health. SAGM, Saline Adenine Glucose Mannitol, is a broadly used additive solution that contains the nutrients and other components vital to red blood cell survival. In SAGM concentrated red blood cells can be stored for up to 42 daysbefore expiry.
Autologous shed red blood cells are returned to a patient within 6 hours after leaving the body.Without intermediate refrigeration. This makes that autologous blood cells typically are healthier and less fragile than stored red blood cells.
Stay tuned to learn more on six other reasons why patients’ own lost blood should be considered for blood transfusion.

Pingback: Bangladeshi donor blood transfusion fails young worker, why we should consider autologous blood - Hemoclear