An estimated 4 million women need a blood transfusion after giving birth annually. Now new research has found that their pregnancies put these women are at a higher risk of adverse transfusion reactions.
In her documentary No woman, no cry Christy Turlington features stories of pregnant women that are afraid to give birth. Unlike these mothers, Christy did not expect that the joy of welcoming her son into the world would abruptly end. Within minutes after the delivery, she went from feeling invincible to powerless. The midwife called for backup and took her baby away, she had started bleeding severely. The fear and panic of that moment, Christy will never forget. Fortunately, she was able to receive proper treatment that saved her life. But she has since learned that each day, for up to 550 women, the postpartum bleeding turns out to be a death sentence.
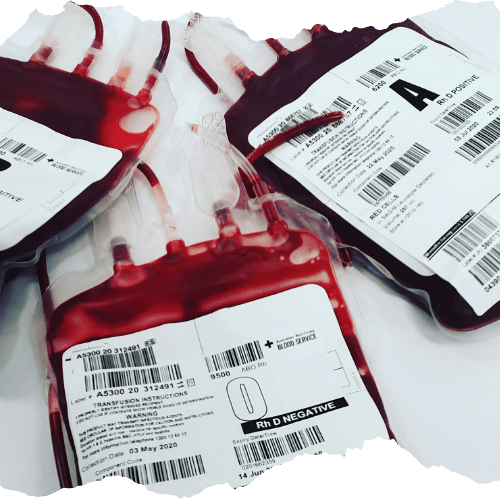
Transfusion Reactions Are Twice As Common In Postpartum Women
Postpartum women are twice as likely to experience a transfusion reaction compared to non-pregnant women. Particularly if they suffer from preeclampsia or go through premature delivery or induced labour. This is what a large retrospective study performed at Karolinska University Hospital in Sweden revealed. Lars Thurn and his colleagues went through the medical records of over half a million pregnant women, and compared these to the records of non-pregnant women that received donor blood to come to their finding.
The exact root of the increased risk remains unknown. During pregnancy the levels of platelet, as well as erythrocyte-leukocyte antibodies increase. Leukocyte and human leukocyte antigen (HLA) antibodies are both associated with various types of transfusion complications. However the level of HLA antibodies increases with additional pregnancies. But an increase in reaction risk as the number of women’s had more previous pregnancies was not revealed.
Another theory focuses on blood pressure. Both in transfusion-related acute lung injury (TRALI) and transfusion-associated circulatory overload (TACO) the endothelium is damaged. Preeclampsia occurs more often during later stages of pregnancy and is known to affect the endothelium of the blood vessels. Which according to Thurn might not be a coincidence.
Autologous Transfusion Is Fundamental To Avoid Transfusion Complications
Transfusion-related adverse events fortunately are rare, but do contribute to maternal morbidity and mortality. Thurn’s research – and the consideration that pregnant women account for a large portion of blood transfusion – once again stress the need for effective strategies to minimize the exposure to allogenic blood components and avoid transfusion reactions. To this end using patients’ own, maximally compatible blood for autologous transfusion is key.
Follow HemoClear on social media to learn more on six other reasons why we have to consider patients’ own lost blood for blood transfusion.